Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
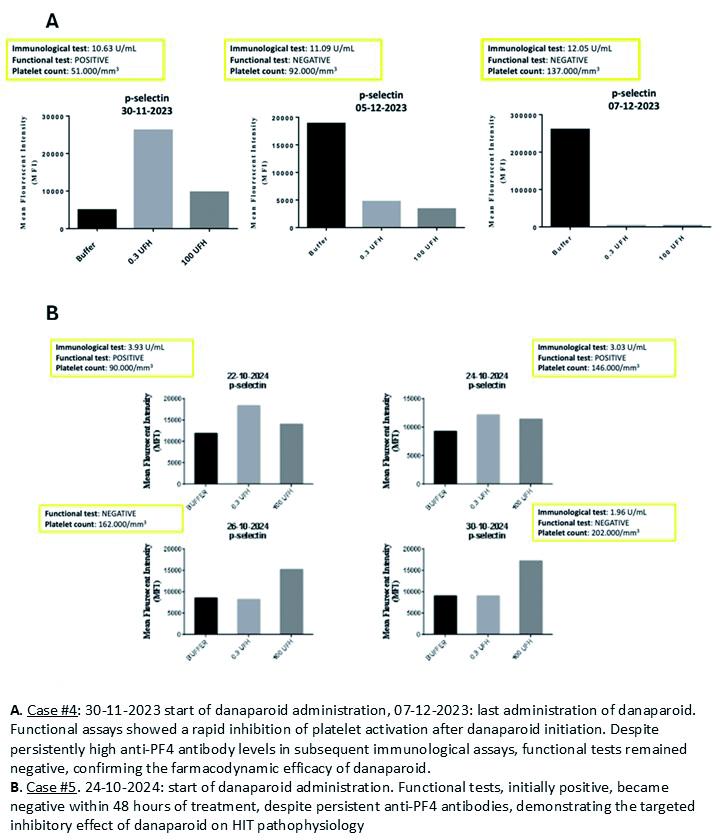
PO80 | Heparin-induced thrombocytopenia: a monocentric experience with danaparoid
L. D’Innocenzo, S. Sorrentino, M. De Siati, A. Ferretti, E. De Candia | Unit of Haemostasis and Thrombosis Diseases, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Roma, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
454
Views
0
Downloads
Similar Articles
- PO44 | Emicizumab in acquired haemophilia A , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO72 | Fondaparinux in patient with active tuberculosis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO10 | Clinical and laboratory features of long-Covid syndrome: a cross-sectional study of 1,337 Covid-19 survivors , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO45 | Routine prophylaxis with PD-FX concentrate in severe inherited FX deficiency: a case report , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO73 | False-positive CT diagnosis of DVT in a patient with severe venous sequelae: a case of bilateral cellulitis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO11 | Neutrophil cathepsin G and risk of cardiovascular events in patients with diabetes mellitus , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO01 | Diagnosis of inherited platelet function disorders by platelet aggregometry using a fully automated coagulation analyzer , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO74 | Combined therapeutic approaches in a patient with hereditary hemorrhagic telangiectasia (HHT) and cardiovascular comorbidities , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO12 | Characterisation and real word clinical data of HEM006, a newly formulated intranasal spray desmopressin (DDAVP) to address a global treatment gap , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO02 | Pregnancy and delivery in women with hemophilia and carriers are still challenging: a ten years analysis from The Italian Association of Hemophilia Centers (AICE) , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
1-10 of 96
Next
You may also start an advanced similarity search for this article.