Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
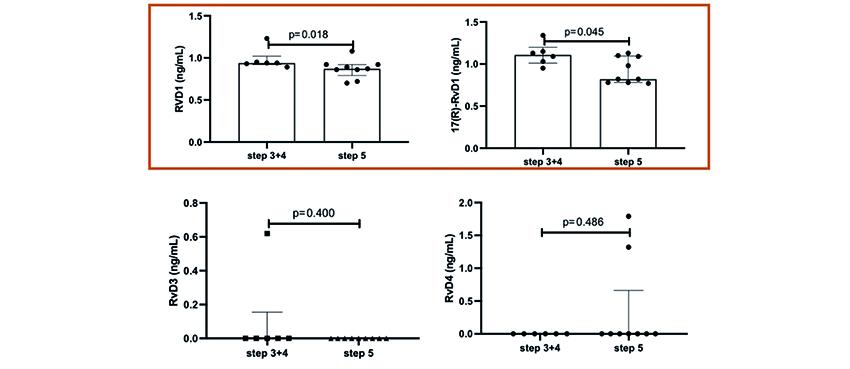
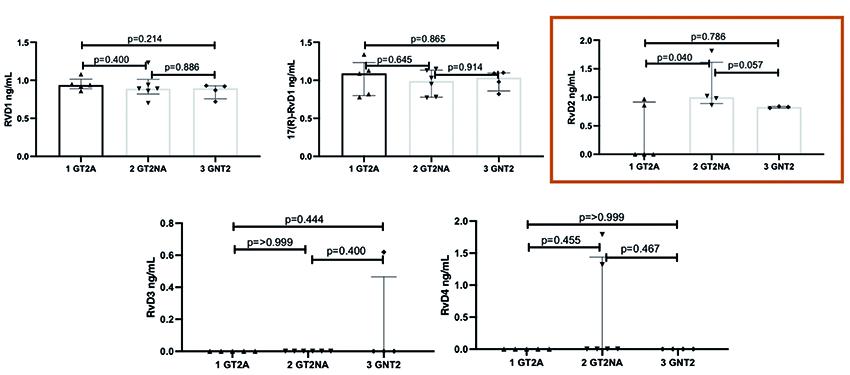
PO54 | Resolvin response in bronchial asthma patients: endotype and clinical severity
R. Liani1, I. Altomare2, P.G.M. Simeone1, M. Alfonsetti1, M. Mucci3, D. Madonna1, S. Lattanzio1, A. Ricci4, A.M. Draicchio2, A. De Sanctis2, P. Di Mattia2, F. Papa2, E. Cavallucci2, F. Cipollone1, A. Recchiuti3, F. Santilli1 | 1Department of Medicine and Aging, and Center for Advanced Studies and Technology “CAST”, G. d’Annunzio University of Chieti-Pescara, Chieti; 2Allergy and Immunology Section, Department Internal Medicine, G. d’Annunzio University, School of Medicine, Chieti; 3Department of Medical, Oral and Biotechnological Sciences, and Center for Advanced Studies and Technology “CAST”, G. d’Annunzio University, Chieti-Pescara; 4Department of Pharmacy, University G. d’Annunzio of Chieti Pescara, Chieti, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
370
Views
0
Downloads