Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
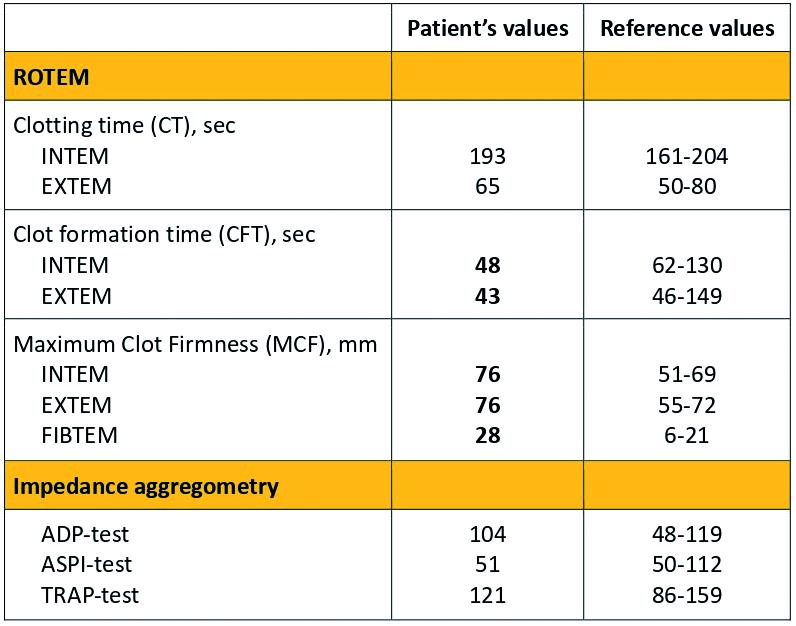
PO68 | Whole blood hypercoagulable profiles in a patient with markedly elevated lipoprotein(A) plasma levels and thrombotic complications: a case report
C. Portinari, M. Biolo, A. Napolitano, L. Spiezia, A. Colpo, S. Zambon, A. Zambon, P. Simioni | Department of Medicine, Padova University Hospital, Padova, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
414
Views
0
Downloads
Similar Articles
- PO46 | Intravitreal treatment with faricimab in patients with age-related macular degeneration , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO79 | Trying to hit the hit in the shadow of renal failure: a complex case managed with danaparoid , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO18 | Does muscle mass matter? Appendicular lean mass as a determinant of anti-XA activity in elderly patientes , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO47 | Hemophilia A and antithrombin deficiency: a case of natural hemostatic rebalancing , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO80 | Heparin-induced thrombocytopenia: a monocentric experience with danaparoid , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO19 | Joint health status in patients with moderate hemophilia A: a cross-sectional multi-center study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO48 | Thrombotic risk evaluation and thrombophilia testing in β-thalassemia patients: a retrospective cohort analysis from a reference regional center , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO81 | Direct oral anticoagulants in atypical site vein thrombosis: a single centre experience focused on cancer patients , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO20 | Impact of endovascular treatment on functional outcome in ischemic stroke: a real-world retrospective study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO49 | Use of emicizumab in two patients with acquired hemophilia A: a new therapeutic approach , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
1-10 of 96
Next
You may also start an advanced similarity search for this article.