Editorials
Vol. 1 No. 2 (2022)
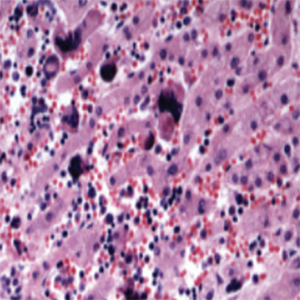
Clonal hematopoiesis and inflammation: a link with thrombosis and malignancy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Received: 9 May 2022
Accepted: 4 July 2022
Accepted: 4 July 2022
3018
Views
357
Downloads
Similar Articles
- PO51 | Thrombocythemia associated with a non-canonical JAK2 mutation: a case report , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO35 | Cerebral veins thrombosis in patients with and without myeloproliferative neoplasm: a real life retrospective monocentric study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO25 | Thromboinflammation and ros accumulation in individuals with high lipoprotein(a) levels , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO09 | Comparison of different aggregometry methods for evaluation of platelet function in patients with myeloproliferative neoplasms , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO56 | Safety of anticoagulant treatment in patients with splanchnic vein thrombosis and history of portal hypertension-related bleeding , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO26 | Non-canonical coagulation platelets function: monocyte-platelet interaction a bridge between inflammation and coagulation , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO06 | Extracellular vesicles profiles in patients with porto-sinusoidal vascular disease , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO84 | Beyond the scores: unmasking a silent pulmonary embolism in essential thrombocythemia , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- Roger Lijnen, Désiré Collen, The key to fibrinolysis and thrombolysis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
- Renato Marino, Silvia Linari, Marzia Leotta, Antonio Coppola, Chiara Biasoli, Maria Elisa Mancuso, Flora Peyvandi, Cristina Santoro, Ezio Zanon, Rita Carlotta Santoro, Diagnostic and management practices for inherited fibrinogen disorders: a nationwide survey of Italian Hemophilia Treatment Centers , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
1-10 of 212
Next
You may also start an advanced similarity search for this article.