Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
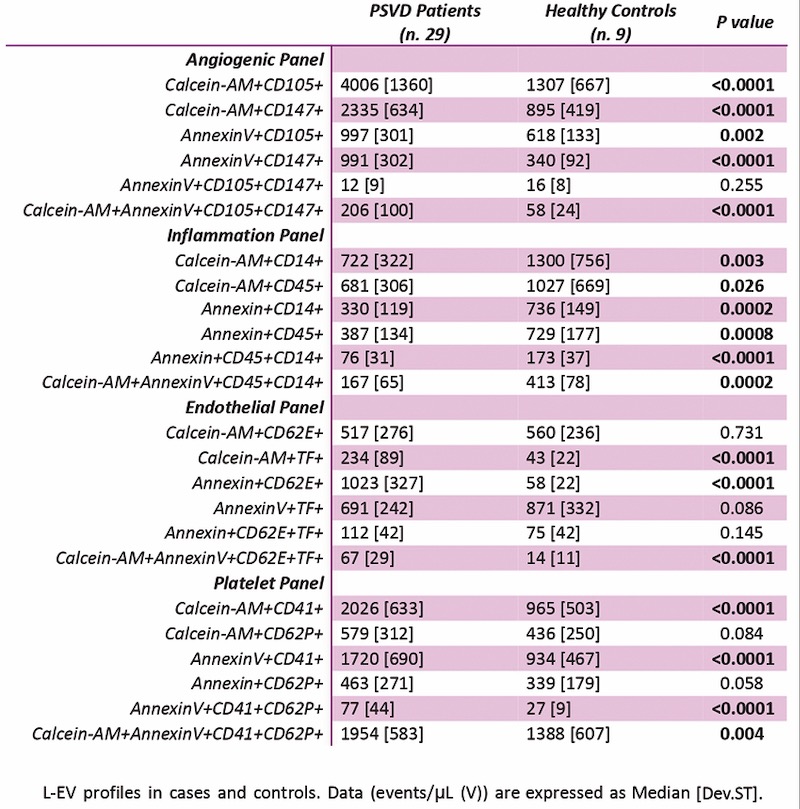
PO06 | Extracellular vesicles profiles in patients with porto-sinusoidal vascular disease
S. Toffanin1, E. Campello1, A. Zanetto2, C. M. Radu1, E. Pinto2, K. Fernande2, C. Bulato1, B. Serena1, L. Spiezia1, P. Burra2, M. Senzolo2, P. Simioni1 | 1First Chair of Internal Medicine, Department of Medicine, University Hospital of Padua Medical School, Padua; 2Department of Surgery Oncology and Gastroenterology, Gastroenterology and Multivisceral Transplant Unit, University Hospital of Padua, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
369
Views
0
Downloads
Similar Articles
- PO37 | Single centre experience on anticoagulation in carriers of non-mild inherited thrombophilia: direct oral anticoagulants (DOAC) efficacy and safety , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO65 | Utilization of emicizumab in acquired hemophilia A: a case report , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- Guest Editor: Valerio De Stefano, 29th National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, 2025 , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO38 | Rates of hemorrhagic events and hemodialysis circuit thrombosis in patients with end-stage renal disease on hemodialytic treatment receiving a factor-XI inhibitor: a systematic review and meta-analysis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO66 | Viscoelastic tests in disseminated intravascular coagulation associated with aortic aneurysm , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO03 | Enlarged platelets with reduced GP IB/IX can indicate disorders other than Bernard-Soulier syndrome , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO39 | Bleeding events in Von Willebrand disease type 1 yearly treatable with desmopressin , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO67 | Pancreatic cancer in a 71-year-old severe hemophilia A patient with inhibitors and sustained zero bleeding during emicizumab prophylaxis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO04 | Classification criteria for antiphospholipid syndrome: ACR/EULAR 2023 versus Sydney 2006 – A monocentric and retrospective study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO40 | Management of paediatric patients affected by mild factor VII deficiency undergoing surgery , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
1-10 of 96
Next
You may also start an advanced similarity search for this article.