Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
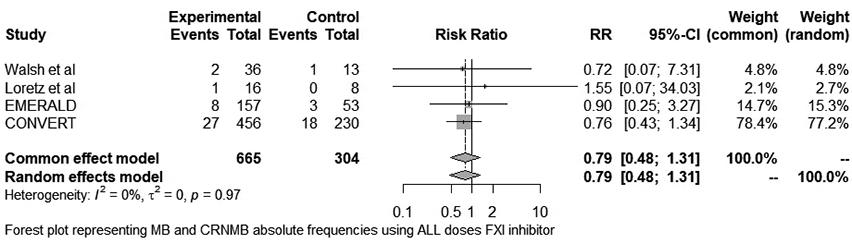
PO38 | Rates of hemorrhagic events and hemodialysis circuit thrombosis in patients with end-stage renal disease on hemodialytic treatment receiving a factor-XI inhibitor: a systematic review and meta-analysis
D. Santagata, G. Barbui, M.P. Donadini, A. Squizzato | Department of Medicine and Surgery, Research Center on Thromboembolic Disorders and Antithrombotic Therapies, University of Insubria, Varese and Como, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
386
Views
0
Downloads
Similar Articles
- PO08 | Efficacy and safety of thromboprophylaxis in hospitalized hematological patients: a monocenter retrospective study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO43 | Extended treatment with reduced dose of direct oral anticoagulants in patients with venous thromboembolism: a retrospective study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO71 | How the presence of paraproteins can interfere in coagulation tests: case report , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO09 | Comparison of different aggregometry methods for evaluation of platelet function in patients with myeloproliferative neoplasms , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO44 | Emicizumab in acquired haemophilia A , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO72 | Fondaparinux in patient with active tuberculosis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO10 | Clinical and laboratory features of long-Covid syndrome: a cross-sectional study of 1,337 Covid-19 survivors , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO45 | Routine prophylaxis with PD-FX concentrate in severe inherited FX deficiency: a case report , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO73 | False-positive CT diagnosis of DVT in a patient with severe venous sequelae: a case of bilateral cellulitis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO11 | Neutrophil cathepsin G and risk of cardiovascular events in patients with diabetes mellitus , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
1-10 of 96
Next
You may also start an advanced similarity search for this article.