Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
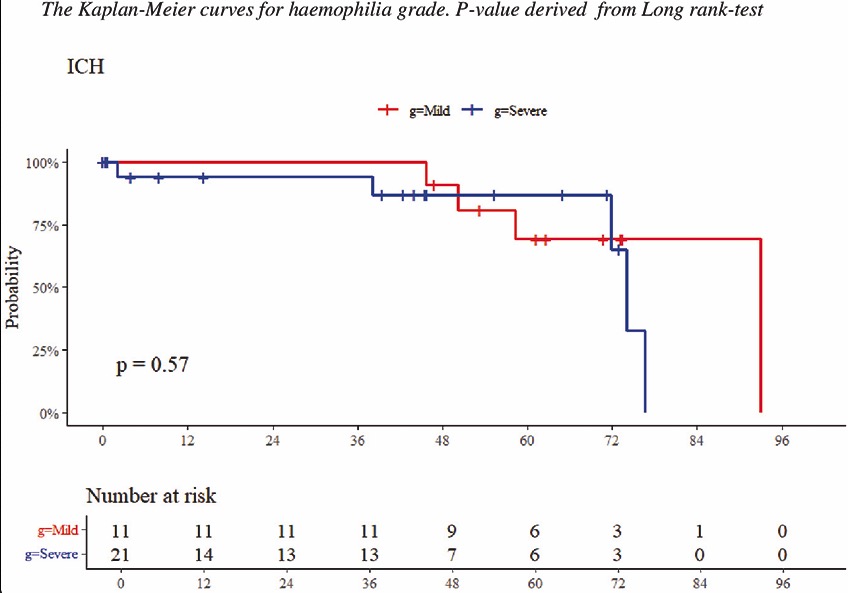
CO27 | Intracerebral hemorrhage in hemophilia A and B: a 10-year prospective multicenter study in Italy (2012–2022)
E. Zanon1, A. Napolitano1, A. Porreca2, F. Demartis3, A. Coppola4, C. Santoro5, I. Cantori6, A. C. Molinari7, C. Biasioli8, M. Luciani9, G. Sottilotta10, B. Pollio11, A. Borchiellini12, A. Tosetto13, P. Flora14, P. Simioni1 | 1Haemophilia Center, First Chair of Internal Medicine, Department of Medicine, University-Hospital of Padua Medical School, Padua; 2Department of Human Sciences and Promotion of the Quality of Life, Unit of Clinical and Molecular Epidemiology IRCCS San Raffaele Roma Open University, Roma; Unit of Clinical and Molecular Epidemiology IRCCS San Raffaele, Roma; 3Centre for Bleeding Disorders, Careggi University Hospital of Firenze; 4Azienda Ospedaliero Universitaria di Parma; 5Hematology Division, Umberto I University Hospital of Roma; 6Haemophilia Center, Department of Transfusion Medicine, Hospital of Macerata; 7IRCCS Istituto Giannina Gaslini, Genova; 8Haemophilia and Transfusion Centre, Bufalini Hospital, Cesena; 9Children’s Hospital Bambino Gesù, Roma; 10Haemophilia Center, Department of Onco-Hematology and Radioterapy, Hospital of Reggio Calabria; 11Haemophilia Pediatric Center, Transfusion Medicine, City of Health and Science of Turin; 12City of Health and Science of Turin; 13Hemorrhagic and Thrombotic Diseases Unit, S. Bortolo Hospital of Vicenza; 14RCCS Foundation Ca’ Granda Maggiore Policlinico Hospital, Milan, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
437
Views
0
Downloads
Similar Articles
- Silvia Linari, Renato Marino, Marzia Leotta, Antonio Coppola, Patrizia Di Gregorio, Augusto Bramante Federici, Flora Peyvandi, Cristina Santoro, Ezio Zanon, Rita Carlotta Santoro, The landscape of rare coagulation factor deficiency management in Italy: a national hemophilia center survey , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
- CO35 | Bleeding phenotype characterization in patients with congenital bleeding disorders: a multigenic approach using next generation sequencing to identify coagulation-modulating variants , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO33 | Acquired hemophilia A in Liguria, Italy: what six years of data reveal , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO38 | Management of pregnancy, delivery, and postpartum in Italian carriers and women with hemophilia A and B , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO36 | Inhibitor titer at diagnosis and clinical course in acquired hemophilia A: a single-center experience , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO37 | Assessment of clotting factor activity and sterility in thawed fresh frozen plasma supplied to helicopter emergency medical services for prehospital transfusion , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO34 | Evaluation of emicizumab concentration and thrombin generation in a cohort of severe hemophilia A patients with and without inhibitor , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO28 | Cognitive, adaptive abilities and behavioral symptoms in children and adolescents with hemophilia: a pilot study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO30 | Joint prosthetic surgery in patients with hemophilia A: clinical-functional outcomes and quality of life , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO31 | Immune system profiling in FVIII-treated and emicizumab-treated pediatric HA patients , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
1-10 of 133
Next
You may also start an advanced similarity search for this article.