Reviews
Vol. 4 No. 2 (2025)
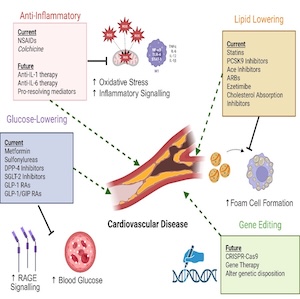
The subtle red line between combating and resolving inflammation in the cardiovascular disease, a “silent sniper”
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 30 June 2025
1122
Views
210
Downloads
Similar Articles
- Alice Lipari, Esmeralda Capristo, Antonietta Ferretti, Erica De Candia, Anticoagulation in obese patients: challenges and strategies , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
- CO25 | Thromboinflammation and ros accumulation in individuals with high lipoprotein(a) levels , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO91 | Disseminated intravascular coagulation with deep vein thrombosis in a frail patient: an extreme manifestation triggered by sepsis during SGLT2i therapy , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO13 | Genetic background in hypercholesterolemic patients framing cardiovascular risk , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- Emanuele Valeriani, Arianna Pannunzio, Danilo Menichelli, Domenico Prisco, Walter Ageno, Daniele Pastori, Pasquale Pignatelli, Executive summary of the SISET position paper on the management of antithrombotic therapy in left ventricular thrombus , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
- Martina Berteotti, Walter Ageno, Rossella Marcucci, Andrea Stella, Paolo Zamboni, Romeo Martini, The role of dyslipidemia and gender-related risk factors in the management of patients with abdominal aortic aneurysms: a survey from the Italian Society of Angiology and Vascular Medicine and a call to action , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 2 (2025)
- CO45 | Role of urinary 11-dehydro-thromboxane B2 as a predictor of preeclampsia in pregnant high-risk women on low-dose aspirin treatment , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- PO32 | Effect of the sodium-glucose co-transporter-2 (SGLT2) inhibitors on platelet activation and lipid peroxidation: results of a pilot study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO18 | Relationship between gut permeability and PCSK9 in heterozygous familial hypercholesterolemia , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO42 | Oxidative stress may contribute to enhanced thrombopoiesis through miR-150: implications for aspirin response , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
1-10 of 147
Next
You may also start an advanced similarity search for this article.