Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
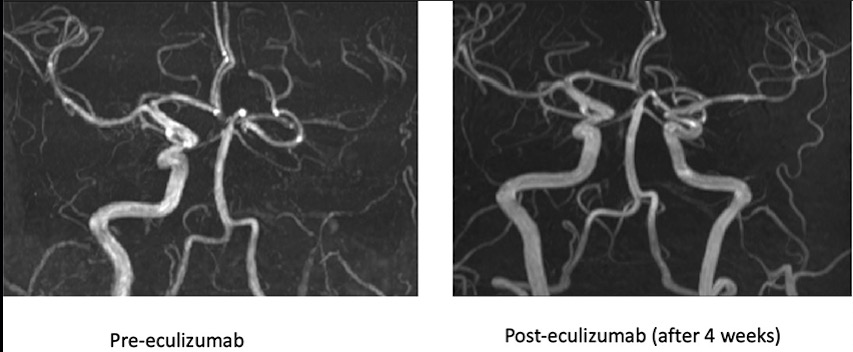
CO12 | Left internal carotid artery thrombosis in a patient with antiphospholipid antibody syndrome successfully treated with eculizumab
A. Hoxha1, L. Nico2, F. Viaro3, L. Fabris1, Y.F. Herrera1, M. Munari4, C. Baracchini3, F. Causin2, P. Simioni1 | 1Internal Medicine Unit, Thrombotic and Haemorrhagic Centre, Department of Medicine - DIMED, University of Padua; 2Neuradiology Unit, University Hospital of Padua; 3Stroke Unit, Neurology Department, University of Padua; 4Intensive Care Unit, University Hospital of Padua, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
429
Views
0
Downloads
Similar Articles
- Alice Lipari, Esmeralda Capristo, Antonietta Ferretti, Erica De Candia, Anticoagulation in obese patients: challenges and strategies , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
- CO09 | Long term effectiveness and safety of direct oral anticoagulants in patients with factor V Leiden and/or prothrombin gene mutation and venous thromboembolism: a single centre, retrospective cohort study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO13 | Genetic background in hypercholesterolemic patients framing cardiovascular risk , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO10 | Multidimensional risk assessment of venous thromboembolism: an observational study comparing the Padua prediction score, Barthel index, and quality of life in hospitalized patients , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO05 | Long-term management of upper extremity catheter-related thrombosis in female patients with cancer: a retrospective cohort study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO06 | Recurrences of catheter associated upper extremity deep vein thrombosis in cancer: a two year prospective study with enoxaparin , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO03 | Early discharge and home treatment of low-risk pulmonary embolism: a cohort study , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO08 | The utility of urine qualitative assessment for direct oral anticoagulants in routine clinical practice , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO04 | Direct oral anticoagulants in antiphospholipid syndrome: a single center real-life experience , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CO02 | Hepatic fibrosis as predictor of cancer-associated thrombosis in patients with intrahepatic cholangiocarcinoma , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
1-10 of 155
Next
You may also start an advanced similarity search for this article.