Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Vol. 4 No. s1 (2025)
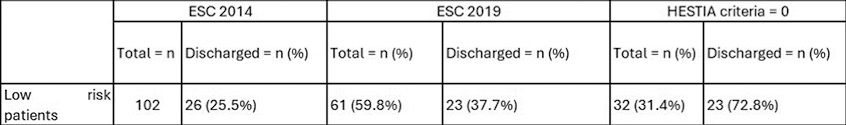
CO03 | Early discharge and home treatment of low-risk pulmonary embolism: a cohort study
E. Ruggeri1, L. Vulcano1, W. Ageno2, F. Cortellaro3, M.P. Donadini3,4 | 1Scuola di Medicina, Università degli Studi dell’Insubria, Varese; 2Dipartimento di Medicina, Università degli Studi di Padova; 3Pronto Soccorso e Medicina d’Urgenza, Ospedale di Circolo, ASST Sette Laghi, Varese; 4Dipartimento di Medicina e Chirurgia, Università degli Studi dell’Insubria, Varese, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 22 October 2025
435
Views
0
Downloads