Abstracts from the 29^ National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, Bergamo, Italy | 23-25 October 2025
Special issues
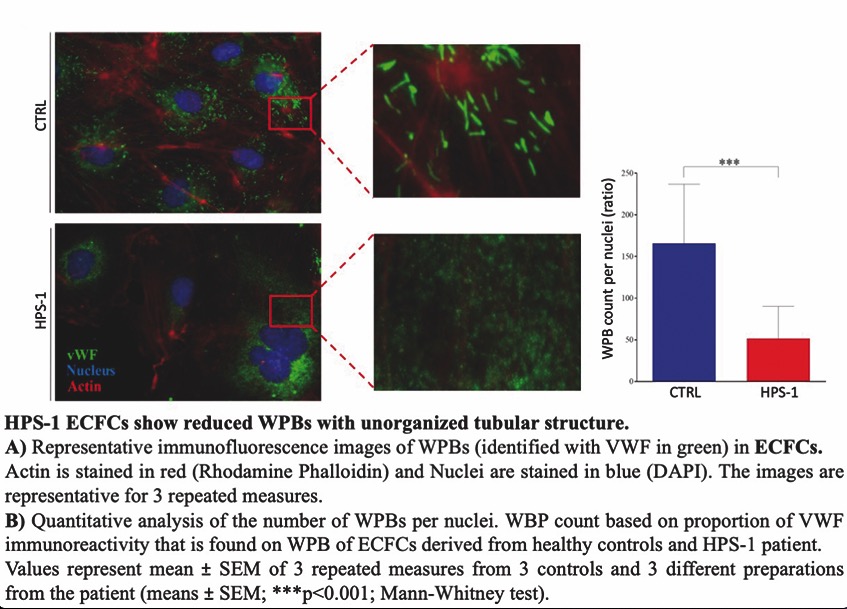
CS07 | Endothelial dysfunction and impaired angiogenesis in Hermansky-Pudlak syndrome (HPS) type 1: studies with endothelial colony forming cells
F. Tondi1, G. Purgatorio1, C. Sgromo2, E. Giglio1, E. Petito1, E. Falcinelli1, G. Guglielmini1, A. Follenzi2, P. Gresele1, L. Bury1*, C. Olgasi3* | *Shared senior authorship; 1Department of Medicine and Surgery, Section of Internal and Cardiovascular Medicine, University of Perugia; 2Department of Health Sciences, School of Medicine, University of Piemonte Orientale, Novara; 3Department of Translational Medicine, School of Medicine, University of Piemonte Orientale, Novara, Italy
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Published: 16 September 2025
209
Views
0
Downloads
Similar Articles
- Guest Editor: Valerio De Stefano, 29th National Conference of the Italian Society for the Study of Hemostasis and Thrombosis, 2025 , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- CS08 | A combination of two rapid immunoassays improves HIT diagnosis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- Silvia Linari, Renato Marino, Marzia Leotta, Antonio Coppola, Patrizia Di Gregorio, Augusto Bramante Federici, Flora Peyvandi, Cristina Santoro, Ezio Zanon, Rita Carlotta Santoro, The landscape of rare coagulation factor deficiency management in Italy: a national hemophilia center survey , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
- Roger Lijnen, Désiré Collen, The key to fibrinolysis and thrombolysis , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
- Bianca Clerici, Mariangela Scavone, Gian Marco Podda, Recent advances in classic heparin-induced thrombocytopenia (HIT), autoimmune HIT, spontaneous HIT, and vaccine-induced immune thrombotic thrombocytopenia , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. 2 (2024)
- CO44 | First interlaboratory validation workshop of immunofluorescence microscopy on the peripheral blood smear for recognizing patients with inherited platelet disorders , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- Luca Puccetti, Vincenzo Sammartano, Federico Caroni, Margherita Malchiodi, Paola Calzoni, Eleonora Franceschini, Lucrezia Galasso, Monica Bocchia, Safety of COVID-19 mRNA vaccination in patients with history of acquired hemophilia A: a case series , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 3 (2022)
- PO03 | Enlarged platelets with reduced GP IB/IX can indicate disorders other than Bernard-Soulier syndrome , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. s1 (2025)
- Marcello Di Nisio, Matteo Candeloro, Nicola Potere, Ettore Porreca, Jeffrey I. Weitz, Factor XI inhibitors: a new option for the prevention and treatment of cancer-associated thrombosis , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. s1 (2024)
- Renato Marino, Silvia Linari, Marzia Leotta, Antonio Coppola, Chiara Biasoli, Maria Elisa Mancuso, Flora Peyvandi, Cristina Santoro, Ezio Zanon, Rita Carlotta Santoro, Diagnostic and management practices for inherited fibrinogen disorders: a nationwide survey of Italian Hemophilia Treatment Centers , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 3 (2025)
1-10 of 140
Next
You may also start an advanced similarity search for this article.